Pay my MedStar Health bill
MedStar Health offers secure, online payment options to make it convenient for you to pay your invoice.
- Pay online through a secure payment portal
- MedStar Health offers fee-free auto phone-pay 24/7. To pay by phone call 410-609-6065 or 855-697-9508.
- Hospital and the majority of all MedStar-employed Physicians’ services all on 1 consolidated statement
- Receive billing statement notifications via text and email
- View and print your statement on-line any time you want
- Pay your bill on-line with extended payment options (Credit card, Healthcare Spending accounts, Apple Pay, Google Pay and ACH check)
- Set up your own recurring payment plans
- Engage in On-line Chat assistance
- Use our Contact Us feature for simple inquiries
Do you need personal assistance with or have questions about your bill?
By calling 410-933-4966 or toll free 844-817-6087, you can reach our Customer Service Division to discuss billing concerns. Representatives are available Monday through Friday, from 8 a.m. to 6 p.m.
Representatives are trained to assist with any questions, concerns or comments that you may have about your bills from MedStar Health, including financial assistance.
Payments and Written correspondence can be mailed to:
MedStar Health Customer Service
PO BOX 411019
Boston, MA 02241-1019
Insurance
Your insurance information will be verified prior to or upon your arrival for services. Please provide any necessary authorizations and/or referrals at the time of service. If the insurance information, authorizations, or referrals are not provided at the time of service, you will be required to sign a financial responsibility form agreeing to pay for the services not covered or denied by your insurance.
If you are insured and undergoing a procedure, the Precertification/Preregistration Department will contact your insurance company prior to services being rendered to secure an estimate of your unmet deductibles and co-insurance amounts. You will then be contacted to make payment arrangements in advance of your procedure.
The final bill for remaining coinsurances and other balances will not be due until MedStar Health has received all payments from your insurance company. You will be billed a consolidated patient balance statement (hospital and the majority of all MedStar-employed physicians). In addition, your insurance carrier(s) will send you statements (explanations of benefits) of their payments made to MedStar Health. These statements also outline any amount for which you may be responsible. Please call your insurance carrier or employer's benefits office for details about your insurance or benefit policy coverage.
If you do not have insurance, you will be notified by your Physician’s office and/or the Precertification/Preregistration Department of the estimated costs and you will be expected to make payment arrangements prior to the time of service.
If you have questions about what services are covered, please check with your health plan or your company's benefits office. They will have the most detailed information about your coverage.
-
Who should I contact if I have a question about my insurance?
Every insurance company has unique policies and procedures, so if you have a question related to your insurance, it’s best to contact your insurance directly. Contact information is located on your health insurance ID card.
If you are eligible for Maryland Medicaid or DC Medicaid, learn more about MedStar Family Choice.
-
How can I tell what my insurance covered?
Final bills are issued only after MedStar Health has received all payments from your insurance provider or providers. Your insurance provider will also send you statements (explanations of benefits) outlining payments made to MedStar Health and any amount for which you may be responsible.
-
Will all of my MedStar Health bills be on one statement?
All hospitals and most employed physician practices will be on the statement, however, you may receive multiple statements for care received during your treatment.
-
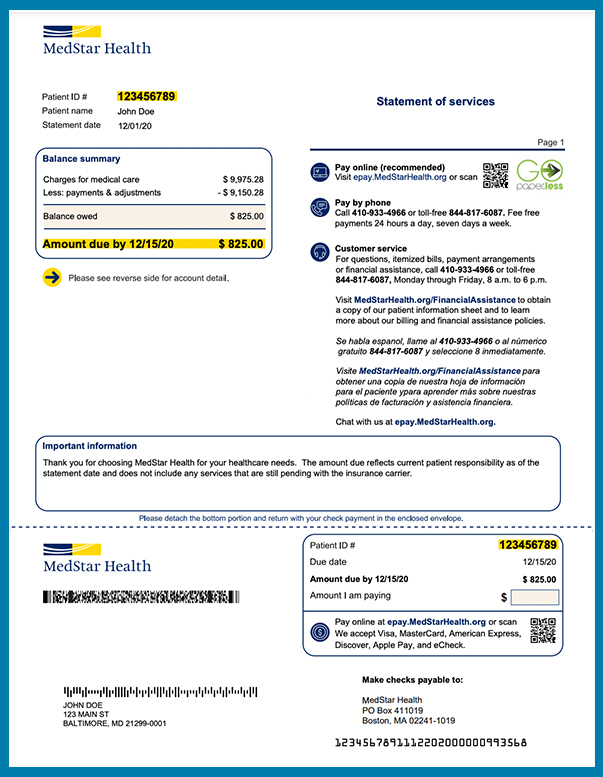
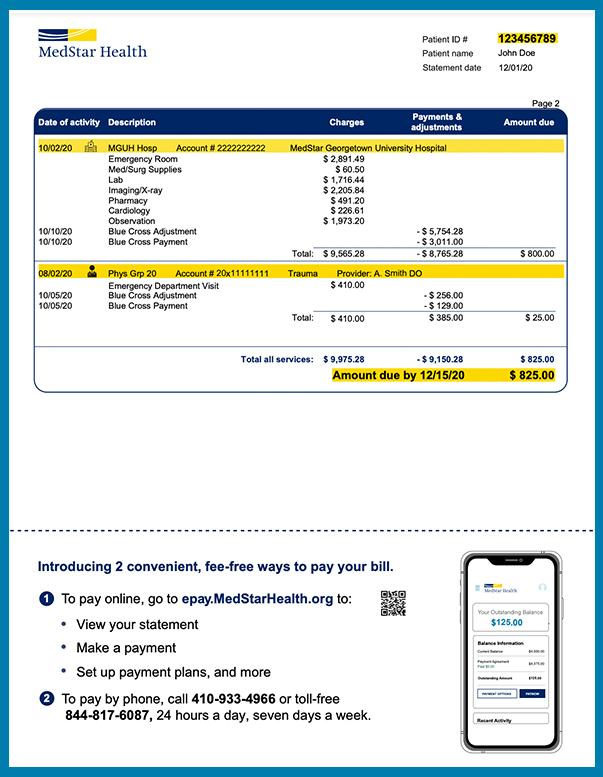
What does a MedStar Health bill look like?
Sample MedStar Health invoice
Front
Back
-
Can I pay my bill by phone?
Yes, MedStar Health offers fee-free auto phone-pay 24/7. Call 410-609-6065 or 855-697-9508 for our pay-by-phone service. -
How do I pay my bill online?
Payments can be made using our secure payment portal.
-
How do I know that my online payment session is secure?
Most browsers will give you a message box stating when you are going into a secure session.
Internet Explorer uses a small padlock icon on the bottom right side of the browser window. When there is a secure session in place, the padlock will appear locked.
Another indication that your browser is operating in secure mode can be found in the website address. The address will begin with "https" - the 's' in 'https' stands for secure./p>
-
What are my obligations to help maintain secure transactions with the ePayments service?
You are responsible for not giving out your bank account information, bank routing information or account information. Be sure to close your browser immediately after you are finished making your payment(s) or updating your account information.
-
When setting up my payment method, where can I find my bank's routing transit number and checking account number?
The routing transit number can be found on the lower left hand side of your check. The checking account number is to the right of the routing number. An illustration is provided when adding or modifying a bank account in Payment Methods.
-
How can I stop the paper bill from being mailed to me when my account is due?
You must be enrolled in the ePayments service in order to stop paper bills from arriving in the mail.
-
How can I contact customer service if I have questions about the ePayments Service?
For information about online statements, payments made via the Internet or any other questions about this service, please contact customer service at 410-933-4966 or toll free 844-817-6087, Monday through Friday, from 8 a.m. to 6 p.m.









