Relieving the pain of pancreatitis
The Chronic Pancreatitis and Autologous Islet Cell Transplant Program at MedStar Health brings hope to those suffering with the debilitating abdominal pain of chronic pancreatitis.
As one of the few centers in the world offering autologous islet cell transplants, patients from throughout the country can find relief from their painful symptoms while reducing or avoiding the complications of diabetes.
Procedure
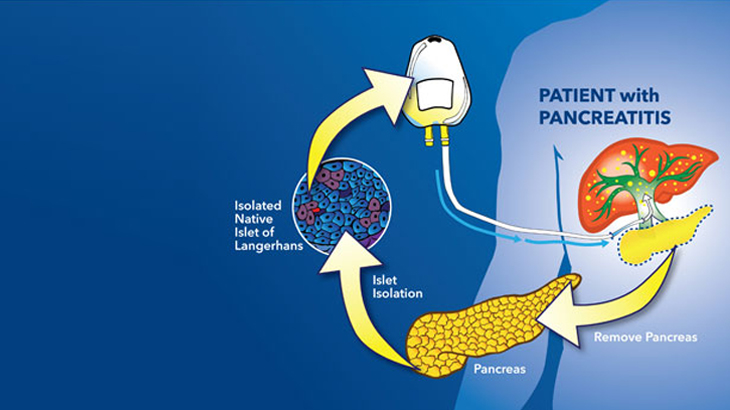
After undergoing complete removal of the pancreas (total pancreatectomy), a patient’s own islet cells (cells that produce insulin) are removed from the pancreas and infused back into the patient’s liver via the portal vein where they take hold and produce insulin.
When the pancreas is removed from a patient in the operating room, it’s immediately put on ice and in a special preserving solution. Once prepared, the pancreas is transported in a cooler to our islet cell lab. There, islet cell scientists work for several hours to separate the islet cells from the pancreas.
Once the islet cells are isolated, they are put into a special solution in an IV bag.
The patient’s islet cells are infused directly into the liver through a catheter, where they can begin functioning and producing insulin.
Specialists
Our Islet Cell Transplant program involves an experienced team of experts from many specialties, including gastroenterology, pain management, endocrinology, and nutrition.
This team is at the forefront of this procedure with extensive clinical experience, research involvement, and an understanding of the frustrations and difficulties those with chronic pancreatitis face. They provide patients compassionate care with access to the most up-to-date treatments.
Evaluation for islet cell transplant
A candidate for the procedure will typically meet these criteria:
-
Severe, debilitating pain that is no longer controlled by medication and may be causing repeated hospitalizations to receive intravenous (IV) pain medication.
-
All other treatment options are exhausted, including endoscopic procedures to treat the pancreatitis.
-
The pancreas still has endocrine function.
If a patient is not a candidate for an islet cell transplant for any reason, the MedStar Health team will identify the best course of treatment to help with symptoms.
Recovery
After the pancreas is removed and the islet cells transplanted into the liver, the patient’s glucose levels are closely monitored. Within 1 to 2 weeks, the islet cells may begin producing insulin.
For 30 to 40 percent of patients, no diabetes develops. However, about 60 to 70 percent will develop diabetes, though it may be less severe than without an islet cell transplant.
It’s important to understand that the process of chronic pancreatitis destroys islet cells so that eventually a patient with chronic pancreatitis may become diabetic, even if the pancreas is never removed.
Most patients (over 90 percent) experience significant pain relief or reduction after the procedure.
Islet cell transplant patients are usually in the ICU for 2 to 4 days after surgery and transplant, with a total hospital stay of 7 to 10 days, followed by several weeks of limited activity to recover at home.
Our providers
Expert surgery care
Getting the care you need starts with seeing one of our surgeons.
Additional information
Transplant Clinic Lab HoursMonday: 7:30 a.m. to 4 p.m.
Tuesday: 7:30 a.m. to 4 p.m.
Wednesday: 9 a.m. to 6 p.m.
Thursday: 7:30 a.m. to 4 p.m.
Friday: 7 a.m. to 3:30 p.m.
Research & clinical trials
Research is a critical part of what we do at MedStar Georgetown University Hospital. Learn more about our research on treating and managing advanced disease and transplantation surgery.
Meet Dr. Khan










